Microbial food poisoning and food infection: a. Food poisoning by: i. Staphylococcus aureus ii. Campylobacter iii. Clostridium botulinum iv. Aspergillus flavus b. Food infection by : i. Salmonella typhimurium ii. Vibrio parahemolyticus
- Get link
- X
- Other Apps
Microbial food poisoning and food infection:
a. Food poisoning by:
i. Staphylococcus aureus
ii. Campylobacter
iii. Clostridium botulinum
iv. Aspergillus flavus
b. Food infection by :
i. Salmonella typhimurium
ii. Vibrio parahemolyticus
Microbial food poisoning and food infection:
Search Results
Featured snippet from the web
a. Food poisoning by:
i. Staphylococcus aureus
Staphylococcus aureus is a gram positive bacterium that usually appears under the microscope as spherical (coccus) organisms appearing in pairs, short chains, or bunched, grape-like clusters.
Staphylococcus aureus has been implicated as a causative agent in acute food poisoning episodes, toxic shock syndrome, impetigo (usually appears as red sores on the face, especially around a child's nose and mouth, and on hands and feet), scalded skin syndrome, cellulitis(The affected skin appears swollen and red and is typically painful and warm to the touch.), folliculitis (common skin condition in which hair follicles become inflamed) and furuncles(is a painful infection that forms around a hair follicle and contains pus).
It is also a common cause of systemic infections such as infective endocarditis(Endocarditis is an infection of the endocardium, which is the inner lining of your heart chambers and heart valves), osteomyelitis (Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Infections can also begin in the bone itself if an injury exposes the bone to germs), epiglottitis(Epiglottitis is inflammation of the epiglottis—the flap at the base of the tongue that prevents food entering the trachea) , and sinus infections( a sinus infection occurs when your nasal cavities become infected, swollen, and inflamed.) amongst others. S. aureus is also responsible for many infective
All people are susceptiblye to infections with Staphylococcus aureus, the disease however, may manifest with varying intensities.
Staphylococcus aureus can cause illness by preformed toxin production as well as by infecting both local tissues and the systemic circulation. Disease transmission can occur in the following settings:
- Gastrointestinal: Staphylococcus aureus causes acute episodes(of short duration ) of food poisoning via preformed enterotoxins. Food items likely to be infected by staphylococcal food poisoning include meat and meat products; poultry and egg products; salads such as egg, tuna, chicken, potato, and macaroni; bakery products such as cream-filled pastries, cream pies, and chocolate éclairs; sandwich fillings; and milk and dairy products.
- Skin and hair infections: Staphylococcus aureus commonly colonizes many skin surfaces on the nasopharynx (the upper part of the pharynx, connecting with the nasal cavity above the soft palate) , and perineum(he perineum is the area between the genitals and the anus); but can cause infection of these surfaces particularly if the cutaneous barrier has been disrupted or damaged.
- Systemic infections: Staphylococcus aureus commonly causes infective endocarditis,osteomyelitis, sinus infections in the general population; and epiglottitis in young children.
- Nosocomial infections: Methicillin resistant Staphylococcal aureus (MRSA) is a strain of the bacteria that is commonly implicated in nosocomial infection . Risk factors for MRSA colonization or infection in the hospital settings include prior antibiotic exposure, admission to an intensive care unit, surgical incisions, and exposure to infected patients.
Incubation Period for foodborne Staphylococcal aureus disease is 1-6 hours.
Diagnosis Staphylococcal aureus gastrointestinal illness can be diagnosed by isolating the preformed toxins from the contaminated food item. Systemic infections are best diagnosed by blood cultures.
Treatment : Staphylococcal aureus are susceptible to beta-lactamase resistant penicillins such as ticarcillin and pipercillin. Vancomycin is the drug of choice for MRSA infections.
ii. Campylobacter
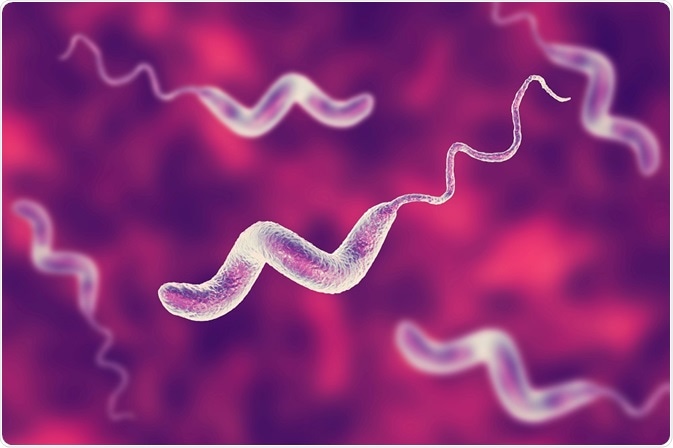
Campylobacter jejuni is a gram negative bacterium most commonly associated with the consumption of undercooked poultry meat and is a common bacterium found in the intestinal tracts of dogs, cats, poultry, swine, cattle, monkeys, wild birds and some humans.
Campylobacter jejuni causes an acute bacterial disease of varying severity that is characterized by diarrhea, abdominal pain, malaise (a general feeling of discomfort, illness) , fever, nausea and vomiting.
Studies indicate that consuming as little as 500 Campylobacter cells can cause disease.
The disease is often associated with gross or occult blood (Fecal occult blood (FOB) refers to blood in the feces that is not visibly apparent) and mucus in liquid stools.
Some of the complications following an acute campylobacter infection can include a typhoid-like syndrome ( Typhoid is a bacterial infection that can lead to a high fever, diarrhea, and vomiting) or reactive arthritis ( is joint pain and swelling triggered by an infection in another part of your body — most often your intestines, genitals or urinary tract. Reactive arthritis usually targets your knees and the joints of your ankles and feet. Inflammation also can affect your eyes, skin and urethra.)and rarely Guillain-Barre syndrome (is a rare disorder in which your body's immune system attacks your nerves) or meningitis (Meningitis is an inflammation of the meninges. The meninges are the three membranes that cover the brain and spinal cord). Some cases of campylobacteriosis may mimic acute appendicitis.
The period of incubation relates directly to the infective dose ingested, but usually 2-5 days with a range of 1-10 days.
This organism is thought to be one of the most common causes of diarrheal illness worldwide. Campylobacter is often the cause of traveler's diarrhea and there is a high incidence rate among children and young adults in developing countries. This foodborne illness is attributed to the consumption of uncooked chicken or pork, unpasteurized milk, and nonchlorinated water and is often seasonal with most cases reported during warmer months.
The diagnosis of this organism is best completed by isolating the organism from a stool sample.
Treatment :This disease is self-limiting and there is no specific recommended treatment other than rehydration and electrolyte replacement. In some cases, physicians prescribe antibiotics such as erythromycin or ciprofloxacin when diarrhea is severe
iii. Clostridium botulinum
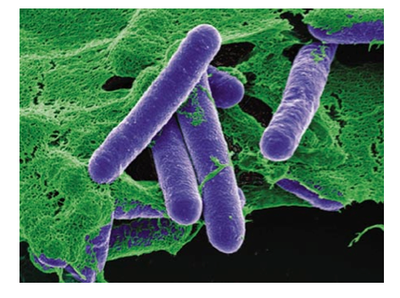
Clostridium botulinum is a Gram-positive, spore-forming, obligate, motile, anaerobic rod shaped bacterium.
Botulism is a serious, but rare intoxication caused by preformed neurotoxins produced by Clostridium botulinum. There are three different forms of botulism:
- Foodborne botulism - Results from ingestion of preformed neurotoxins (Neurotoxins are toxins that are destructive to nerve tissue ), commonly from foods that placed in anaerobic storage such as in cans or jars. Commonly implicated food products are inadequately processed, home canned foods.
- Infant/Intestinal botulism - Usually affects infants and rarely, adults with altered gastrointestinal anatomy or microflora. It is caused by ingesting spores of the botulinum bacteria that multiply in the gut and produce the toxin.
- Wound botulism - Occurs when an open wound is contaminatedj with botulinum spores.
Members of the Clostridium genus are usually ubiquitous in nature. C. tetani releases an exotoxin causing tetanus and lock jaw. C. perfringes is usually acquired from dirt via open wounds. C. perfringes spores produce an exotoxin that causes gas necrosis of the infected area. C. difficile, is usually a part of the normal intestinal flora, and causes disease only when broad spectrum antibiotics such as Clindamycin deplete the other gut microflora. C. difficile then releases exotoxins that cause diarrhea.
Susceptibility is general for both the foodborne and wound botulism. Most patients with infant/ intestinal variety are children between ages 2 weeks and 1 year. Rarely adults with altered gut flora either due to certain diseases, genetic susceptibility or improper antibiotic treatment are also affected.
Botulinum spores are ubiquitous in the soil worldwide. Botulism toxin causes flaccid paralysis ( is a neurological condition characterized by weakness or paralysis) by blocking motor nerve terminals at the myoneural junction. The paralysis progresses in a downward fashion, affecting the eyes and face, throat, chest and extremities and eventually causing respiratory paralysis and death.
Foodborne botulism usually produces neurologic symptoms within 12-36 hours of ingestion, but could also take up to several days. Generally, the shorter incubation periods are associated with severe diseases and higher case-fatality rates.
The history and physical examination is usually the first step in diagnosing botulism. However, nerve conduction studies , spinal fluid examinations and brain scans are helpful. Botulinum bacteria can be isolated from the stool of infected people in the foodborne and infant variety of the disease.
a . Foodborne botulism - If diagnosed early, antitoxin should be administered to block the actions of the exotoxin. If respiratory failure has set in, mechanical ventilator and intensive care is required.
b. Infant botulism - Remove the contaminated food by inducing vomiting . Good supportive care is further required for recovery.
c . Wound botulism - Administration of antitoxins to neutralize the exotoxin, surgical debridement and excision of the effected area, followed by the required supportive treatment
iv. Aspergillus flavus:
Aflatoxins are poisonous substances produced by certain kinds of fungi (moulds) that are found naturally all over the world; they can contaminate food crops and pose a serious health threat to humans and livestock.
Aflatoxins are a family of toxins produced by certain fungi that are found on agricultural crops such as maize (corn), peanuts, cottonseed, and tree nuts. The main fungi that produce aflatoxins are Aspergillus flavus and Aspergillus parasiticus, which are abundant in warm and humid regions of the world
Aflatoxins also pose a significant economic burden, causing an estimated 25% or more of the world’s food crops to be destroyed annually.
Two closely related species of fungi are mainly responsible for producing the aflatoxins of public health significance: Aspergillus flavus and A. parasiticus.
Under favourable conditions typically found in tropical and subtropical regions, including high temperatures and high humidity, these moulds, normally found on dead and decaying vegetation, can invade food crops
Drought stress, insect damage and poor storage can also contribute to higher occurrence of the moulds including in more temperate regions
Several types of aflatoxin (14 or more) occur in nature, but four – aflatoxins B1 , B2 , G1 and G2 are particularly dangerous to humans and animals as they have been found in all major food crops; but most human exposure comes from contaminated nuts, grains and their derived products
Additionally, aflatoxin M1 (AFM1 ), a product of aflatoxin B1 (AFB1 ) metabolism, can be found in milk in areas of high aflatoxin exposure
Subsequently humans may be exposed to this aflatoxin through milk and milk products, including breast milk, especially in areas where the poorest quality grain is used for animal feed
Food crops can become contaminated both before and after harvesting
Pre-harvest contamination with aflatoxins is mainly limited to maize, cottonseed, peanuts and tree nuts
Post-harvest contamination can be found in a variety of other crops such as coffee, rice and spices
Improper storage under conditions that favour mould growth (warm and humid storage environments) can typically lead to levels of contamination much higher than those found in the field
Long-term exposure can have serious health consequences Long-term or chronic exposure to aflatoxins has several health consequences including:
aflatoxins are potent carcinogens and may affect all organ systems, especially the liver and kidneys;
they cause liver cancer, and have been linked to other types of cancer – AFB1 is known to be carcinogenic in humans;
the potency of aflatoxin to cause liver cancer is significantly enhanced in the presence of infection with hepatitis B virus (HBV)
aflatoxins are mutagenic in bacteria (affect the DNA), genotoxic, and have the potential to cause birth defects in children;children may become stunted, although these data have yet to be confirmed because other factors also contribute to growth faltering e.g. low socioeconomic status, chronic diarrhoea, infectious diseases, malnutrition
aflatoxins cause immunosuppression, therefore may decrease resistance to infectious agents (e.g. HIV, tuberculosis);
b. Food infection by :
i. Salmonella typhimurium:
Salmonella infection (salmonellosis) is a common bacterial disease that affects the intestinal tract. Salmonella bacteria typically live in animal and human intestines and are shed through feces. Humans become infected most frequently through contaminated water or food.
Typically, people with salmonella infection have no symptoms. Others develop diarrhea, fever and abdominal cramps within eight to 72 hours. Most healthy people recover within a few days without specific treatment.
In some cases, the diarrhea associated with salmonella infection can be so dehydrating as to require prompt medical attention. Life-threatening complications also may develop if the infection spreads beyond your intestines. Your risk of acquiring salmonella infection is higher if you travel to countries with poor sanitation.
Salmonella infection is usually caused by eating raw or undercooked meat, poultry, eggs or egg products. The incubation period ranges from several hours to two days. Most salmonella infections can be classified as stomach flu (gastroenteritis). Possible signs and symptoms include:
- Nausea
- Vomiting
- Abdominal cramps
- Diarrhea
- Fever
- Chills
- Headache
- Blood in the stool
A few varieties of salmonella bacteria result in typhoid fever, a sometimes deadly disease that is more common in developing countries.
Salmonella bacteria live in the intestines of people, animals and birds. Most people are infected with salmonella by eating foods that have been contaminated by feces. Commonly infected foods include:
- Raw meat, poultry and seafood. Feces may get onto raw meat and poultry during the butchering process. Seafood may be contaminated if harvested from contaminated water.
- Raw eggs. While an egg's shell may seem to be a perfect barrier to contamination, some infected chickens produce eggs that contain salmonella before the shell is even formed. Raw eggs are used in homemade.
- Fruits and vegetables. Some fresh produce, particularly imported varieties, may be hydrated in the field or washed during processing with water contaminated with salmonella. Contamination also can occur in the kitchen, when juices from raw meat and poultry come into contact with uncooked foods, such as salads.
The Food and Drug Administration also indicates that some salmonella outbreaks have been traced to contaminants in spices. The agency is seeking ways to increase the safety of spices.
Many foods become contaminated when prepared by people who don't wash their hands thoroughly after using the toilet or changing a diaper. Infection also can occur if you touch something that is contaminated, including pets, especially birds and reptiles, and then put your fingers in your mouth.
Factors that may increase your risk of salmonella infection include activities that may bring you into closer contact with salmonella bacteria and health problems that may weaken your resistance to infection in general.
Increased exposure
- International travel. Salmonella infection, including varieties that cause typhoid fever, is more common in developing countries with poor sanitation.
- Owning a pet bird or reptile. Some pets, particularly birds and reptiles, can carry salmonella bacteria.
Stomach or bowel disorders
Your body has many natural defenses against salmonella infection. For example, strong stomach acid can kill many types of salmonella bacteria. But some medical problems or medications can short-circuit these natural defenses. Examples include:
- Antacids. Lowering your stomach's acidity allows more salmonella bacteria to survive.
- Inflammatory bowel disease. This disorder damages the lining of your intestines, which makes it easier for salmonella bacteria to take hold.
- Recent use of antibiotics. This can reduce the number of "good" bacteria in your intestines, which may impair your ability to fight off a salmonella infection.
Immune problems
The following medical problems or medications appear to increase your risk of contracting salmonella by impairing your immune system.
- AIDS
- Sickle cell disease
- Malaria
- Anti-rejection drugs taken after organ transplants
- Corticosteroids
Complications
Salmonella infection usually isn't life-threatening. However, in certain people — especially infants and young children, older adults, transplant recipients, pregnant women, and people with weakened immune systems — the development of complications can be dangerous.
Dehydration
If you can't drink enough to replace the fluid you're losing from persistent diarrhea, you may become dehydrated. Warning signs include:
- Decreased urine output
- Dry mouth and tongue
- Sunken eyes
- Reduced production of tears
Bacteremia
If salmonella infection enters your bloodstream (bacteremia), it can infect tissues throughout your body, including:
- The tissues surrounding your brain and spinal cord (meningitis)
- The lining of your heart or valves (endocarditis)
- Your bones or bone marrow (osteomyelitis)
- The lining of blood vessels, especially if you've had a vascular graft
Reactive arthritis
People who have had salmonella are at higher risk of developing reactive arthritis. Also known as Reiter's syndrome, reactive arthritis typically causes:
- Eye irritation
- Painful urination
- Painful joints
You can also take care to avoid spreading bacteria to others. Preventive methods are especially important when preparing food or providing care for infants, older adults and people with weakened immune systems. Be sure to cook food thoroughly and refrigerate or freeze food promptly.
Wash your hands
Washing your hands thoroughly can help prevent the transfer of salmonella bacteria to your mouth or to any food you're preparing. Wash your hands after you:
- Use the toilet
- Change a diaper
- Handle raw meat or poultry
- Clean up pet feces
- Touch reptiles or birds
Keep things separate
To prevent cross-contamination:
- Store raw meat, poultry and seafood away from other foods in your refrigerator
- If possible, have two cutting boards in your kitchen — one for raw meat and the other for fruits and vegetables
- Never place cooked food on an unwashed plate that previously held raw meat
Avoid eating raw eggs
Cookie dough, homemade ice cream all contain raw eggs. If you must consume raw eggs, make sure they've been pasteurized.
Salmonella infection can be detected by testing a sample of your stool. However, most people have recovered from their symptoms by the time the test results return.
If your doctor suspects that you have a salmonella infection in your bloodstream, he or she may suggest testing a sample of your blood for the bacteria.
- Anti-diarrheals. Medications such as loperamide (Imodium A-D) can help relieve cramping, but they may also prolong the diarrhea associated with salmonella infection.
- Antibiotics. If your doctor suspects that salmonella bacteria have entered your bloodstream, or if you have a severe case or a compromised immune system, he or she may prescribe antibiotics to kill the bacteria. Antibiotics are not of benefit in uncomplicated cases. In fact, antibiotics may prolong the period in which you carry the bacteria and can infect others, and they can increase your risk of relapse.
ii. Vibrio parahemolyticus

Vibrio parahaemolyticus is an intestinal infection that is characterized by lower gastrointestinal distress such as diarrhea and cramps. In some cases, nausea, vomiting, fever and headache may also be present.
Occasionally, this disease may manifest itself as a dysentery-like illness with bloody or mucoid stools, high fever and a high white blood cell count, but normally the disease has a duration of only two to three days. Illness with Vibrio parahaemolyticus is most common during the summer months.
This disease is most often associated with eating raw or inadequately cooked seafood or any food contaminated by handling raw seafood or contaminated water. This disease is primarily associated with the consumption of raw oysters.
There are several other bacterium from the vibrio family that may cause diarrheal disease including: V. chloerae (of serogroups other than 01), V. fluvialis, V. furnissii and V. hollisae. Sepiticemic disease associated with wound type infections have been associated with V. hollisae. V. alginolyticus and V. damsela.
The incubation period for Vibrio parahaemolyticus is usually between 12 - 24hours, but can range from 4-96 hours with a mean of 15 hours.
This organism is not communicable from person to person. Cases of Vibrio parahaemolyticus usually occur during the summer months, due to the fact that the organism can be found floating free in coastal waters and in fish and shellfish. During cooler months, the organism is commonly found in silt or mud on the bottom of marine environments.
Vibrio parahaemolyticus is diagnosed by isolating the Kanagawa Vibrio, which is halophilic and is one of the characteristics that produce the hemolytic reaction known as the "Kanagawa phenomenon". There are twelve separate "O" antigen groups and approximately sixty different "K" antigen types that have been identified with this organism. Diagnosis can be determined by the presence of the Kanagawa vibrios in the patient's stool culture or in implicated food.
Symptoms of Vibrio parahaemolyticus infection usually occur within 24 hours (range, 4-96 hours) after ingesting the bacteria.
- Symptoms of Vibrio parahaemolyticus infection may include:
- Watery diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Fever
- Headache
- Bloody diarrhea
Illness typically lasts 1 to 7 days. Treatment is not necessary in most cases. Severe illness is rare and occurs most often in persons with weakened immune systems
This disease is self limiting and best treated with plenty of water replenishment. Antibiotics are usually not necessary but in very sever cases tetracycline, ampicillin or ciprofloxacin could be used.
- Get link
- X
- Other Apps



Comments
Post a Comment